Trust-Based Clinical Alerts
Methodology
- Contextual inquiry
- Survey
Problem Space
Physicians receive drug–drug interaction (DDI) alerts every day, and 96% of those alerts are ignored. Not following these alerts increases the risk of prescribing unsafe medications, which can cause serious health complications and even death. Prior research has focused on improving the design of these alerts but has shown only limited success in increasing adherence.
We proposed a different perspective: instead of starting with redesigning alerts, we focused on improving trust between physicians and computerized alerts by examining why physicians trust their medical colleagues.
Research Question
What are the characteristics of an information source—whether a mentor, a colleague, or the medical literature—that make physicians trust it in their clinical work?
Our Approach
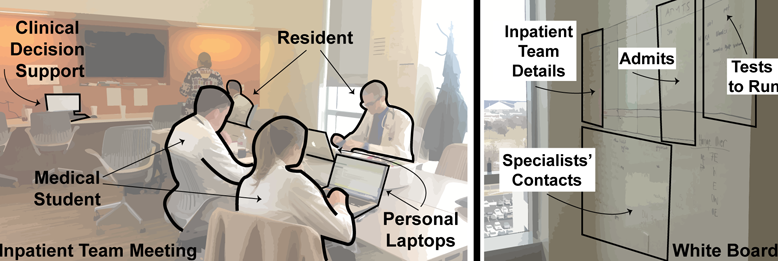
To understand trusted advice among physicians, we conducted three contextual inquiries in a hospital setting with 22 participants and confirmed our findings with a survey of 37 participants.
Impact
- Introduced seven design directions for trust-based alerts to improve physician compliance: Endorsement, Transparency, Team sensing, Collaborative, Empathic, Conflict mitigating, Agency laden
- Contributed to new alert design strategies to improve the effectiveness of drug safety advice
My Responsibilities
- Conducted contextual inquiries and a survey in collaboration with a UX researcher and Principal Investigators
- Analyzed and synthesized findings from the contextual inquiry and survey to inform our design directions
Funding
NSF-funded research project “SCH: EXP: From Critique to Collaboration: A Fundamental Rethinking of Computerized Clinical Alerts”, PI: Dr. Jon Duke, then Dr. Davide Bolchini
Publication
Chattopadhyay, D., Ghahari, R. R., Duke, J., & Bolchini, D.(2015). Understanding Advice Sharing among Physicians: Towards Trust-Based Clinical Alerts.. Interacting with Computers. ![]()